|
Event Website |
https://wcp2023.org/ |
|
Event Name |
2023 WCP |
|
Event Dates |
2-7 July, 2023 |
|
|
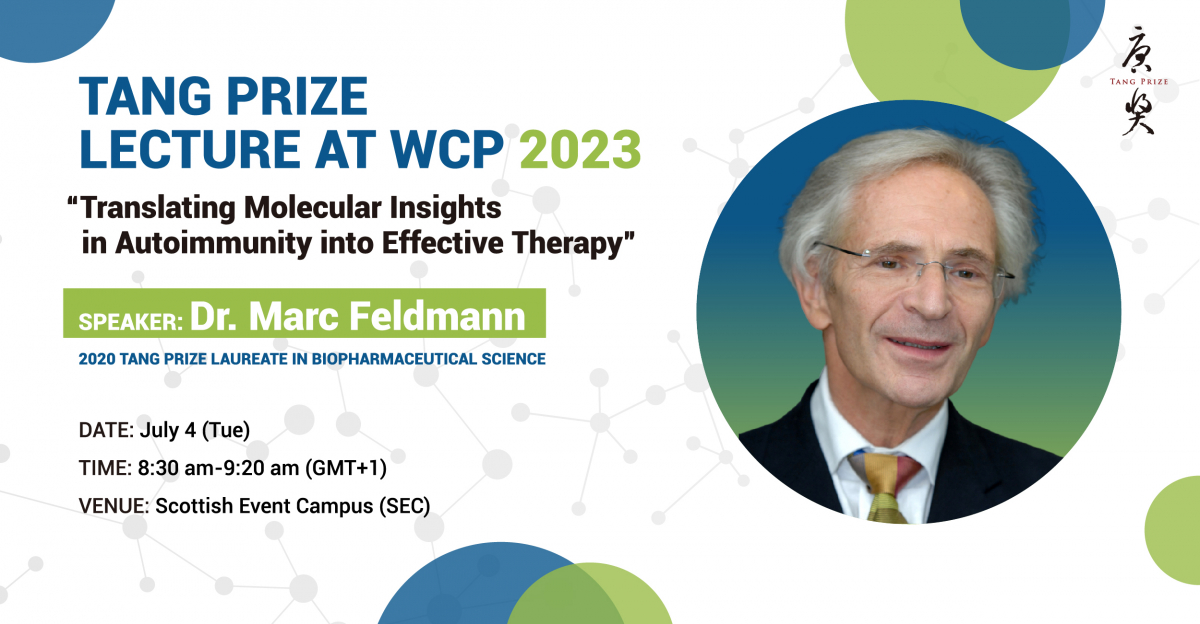
Tang Prize Lecture at 2023 WCP |
|
Time |
8:30-9:20 (GMT+1), July 4, 2023 |
|
Venue |
Online |
|
Speaker |
Professor Marc Feldmann 2020 Tang Prize laureate in Biopharmaceutical Science |
|
Title |
Translating molecular insights in autoimmunity into effective therapy |
|
Abstract |
The molecular mechanism of autoimmunity was elusive until the 1980s-90s. The genetic predisposition mapping to the HLA (major histocompatibility complex) was known in 1970s, but how it enabled immunity was elusive.
Noting the upregulated expression of both MHC class I, and class 2 at multiple autoimmune sites, I proposed that this reflected augmented antigen presenting capacity, and hence an active local immune response. To test this novel idea my colleagues and I used human autoimmune disease tissue, initially from thyroid but later from rheumatoid joints, in order to unravel key mysteries. Most important was which molecular target might facilitate the greatest clinical benefit, for a big unmet need, rheumatoid arthritis which at the time, early 80’s was poorly treated and an increased mortality, a 10 year shorter life span. We used human rheumatoid tissue to elucidate which were the key molecules driving inflammation and tissue destruction. The approach we used was mRNA analysis to detect which mediators were produced locally in joint tissue, and focused on cytokines, at the time newly characterised. It was found that many proinflammatory cytokines were augmented in RA synovial tissue, including IL-1, IL-2, IL-6, IFNg, TNFa, GM-CSF etc. This led to a paradox, if there were many inflammatory cytokines involved, which, if any might be a therapeutic target? Competing research groups abandoned this field, having decided that blocking any one cytokine was unlikely to be beneficial, as inflammation would still be driven by the remaining cytokines. Human synovial tissue, cultured effectively produces cytokines for over a week, providing a test bed for testing antibodies to define potential therapeutic targets. Blocking TNF was found to also diminish the production of other important pro-inflammatory cytokines such as IL-1, IL-6 and GM-CSF, leading to the new concept of the “ TNF dependent cytokine cascade”, and predicting the clinical efficacy of TNF blockade, using antiTNF. Clinical trials are often slow and expensive, because of the need to detect a difference in a heterogeneous population of patients often requires many patients. As often only a fraction benefit from a treatment, and if the degree of benefit is small it may be hard to know if a trial of a new treatment has worked. This was not an issue with trial of the first antiTNF, now sold as infliximab. The 8 patients in the first trial all responded well, both clinically in signs and symptoms, with rapid reduction of fatigue, pain, joint swelling etc. And so if the clinical effect is large, the trials can be smaller and quicker: phase 2 was just 72 patients, phase 3 less than 500.
It is important to remember that infliximab was the first successful monoclonal antibody used in a common disease, long term. And so it led to a therapeutic revolution. As Centocor allowed Ravinder Maini and I to disclose the efficacy revealed in trials prepublication, it allowed other companies to join the race to develop antiTNF monoclonals, and opened up the field, to the great benefit of patients but also of the Pharmaceutical industry. They had a new type of therapeutic, and invested heavily in monoclonal antibody therapeutics. This also led to the boom in anticancer antibodies, initiated by trastuzumab, anti HER2.
Progress in this field will be discussed. |